Treatment Options for Endometrial Cancer
Endometrial Cancer Specialist in Valencia, Spain.
We make a diagnosis based off of the symptoms that indicate that a patient may suffer from endometrial cancer.
If the diagnosis reveals endometrial cancer, you will likely be referred to a trained Gynecologic Oncologist specialist to complete the treatment process as soon as possible.
What is uterine/endometrial cancer?
Endometrial cancer is a disease in which some cells of the body grow uncontrollably.
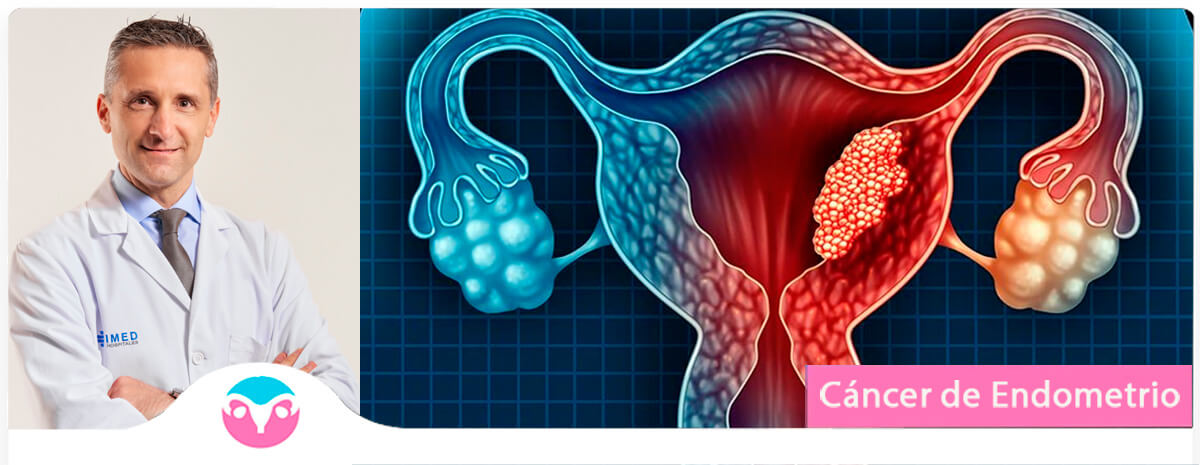
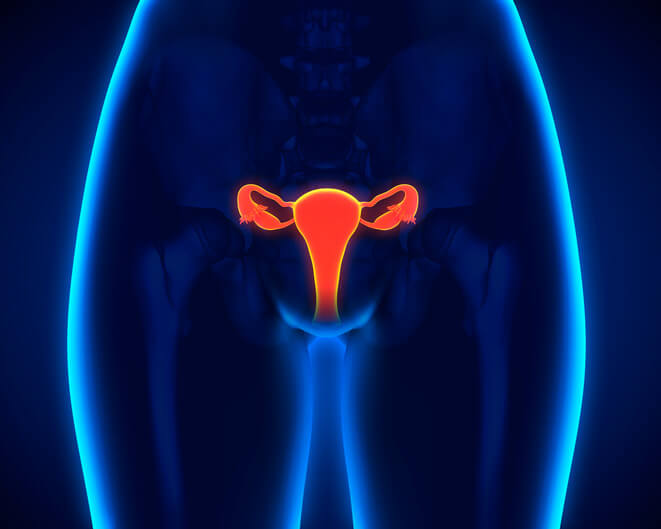
Uterus and endometrium
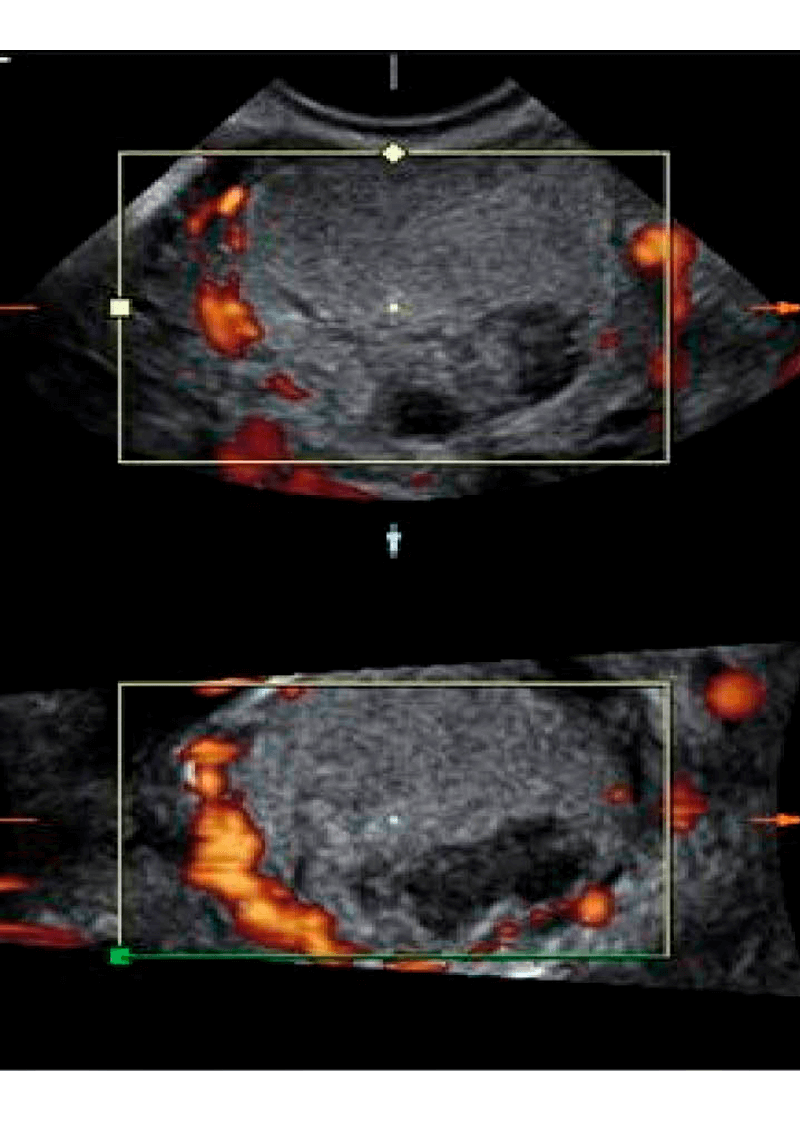
The uterus (or womb) has the function of allowing the embryonic-fetal growth during pregnancy, and is formed by three layers:
- The internal layer is called the endometrium and is what sheds with every menstrual cycle in the form of bleeding during a woman’s fertile years.
- The middle layer is called the myometrium and is composed of actual uterine muscle, is the thickest layer, and is what gives the organ its shape.
- Lastly, the external layer is a thin one and covers the organ (peritoneum).
Types of Endometrial Cancer
Two main types of endometrial cancer are described based on how the cells grow:
-
- The ones that develop from the endometrium, which is the most common of the two.
- The ones that originate from the myometrium, or uterine sarcomas.
Diagnosis: Endometrial Cancer
Almost 80% of women with endometrial cancer are diagnosed in the early stages, and generally, after symptoms appear.
That is why is women must adequately understand the main symptoms of endometrial cancer:
Endometrial cancer symptoms
The signs and symptoms of endometrial cancer, also known as uterine cancer, can include the following:
What are the symptoms of uterine/endometrial cancer?
- Abnormal genital bleeding (the most frequent symptom): This can happen during menopause, or in women of childbearing age between menstrual periods.
- Abnormal vaginal discharge.
- Pelvic pain or a pressure sensation in the pelvic region.
- Changes in intestinal habits or urination..
While these symptoms are also explicable by other causes, women who present any of them persistently should visit the gynecologist.
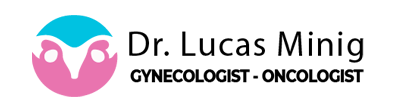
What procedures can help diagnose Endometrial Cancer?
What are the risk factors for developing endometrial cancer?
Most uterine tumors are diagnosed in women approaching menopause, either some years before or after. Around 4.000 women are diagnosed with uterine cancer each year. This is the most frequent gynecologic cancer and the 3rd most common cause of cancer among women.
Even though it is hard to find a specific cause of endometrial cancer, these are some of the main risks factors that could increase the risk of developing it::
- Age: more than 90% of endometrial tumors develop in women more than 40 years of age
- Obesity
- Diabetes
- Hypertension
- Hormone replacement therapy during menopause (with estrogen without progestin)
- Tamoxifen: a drug used in women with certain types of breast cancer that can produce continuous growth of the endometrium.
- Having relatives with a history of uterine, colon, or ovarian cancer.
Having any of the risk factors mentioned does not mean that the woman will have endometrial cancer in the future; it just means it is necessary to talk about it with her gynecologist.
Endometrial cancer prevention
Can endometrial cancer be prevented? Can endometrial cancer be detected early?
There are no effective methods for the prevention or diagnosis of endometrial cancer. The most important factor is that women stay vigilant of the symptoms that can appear and visit a gynecologist as soon as possible for a timely diagnosis and treatment.
The main symptom is genital bleeding after women’s menopause. Pelvic pain or other unspecific symptoms are rare in this type of tumor. Moreover, it is relevant to mention that it is common to make the diagnosis in asymptomatic women.
Endometrial cancer is often associated with gene mutations that can cause cancer in other organs such as the bowel. This is known as Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer) and this is one of the main reasons why women with endometrial cancer must be studied and treated by professionals with enough training and knowledge about this condition.
It is important to remember that pap smears are not useful for the early diagnosis of endometrial cancer. Its role relies on the detection of premalignant lesions in the uterine cervix, or cervical cancer at very early stages.
What do
I have to do to prevent uterine/endometrial cancer?
While there are no specific ways to prevent uterine cancer, some of the following measures might help reduce the risk:
- Oral contraceptives use
- Multiple pregnancies
- Maintaining a healthy and active life with a balanced diet, avoiding obesity, diabetes, and hypertension.
Treatment for uterine cancer:
How must uterine/endometrial cancer be treated?
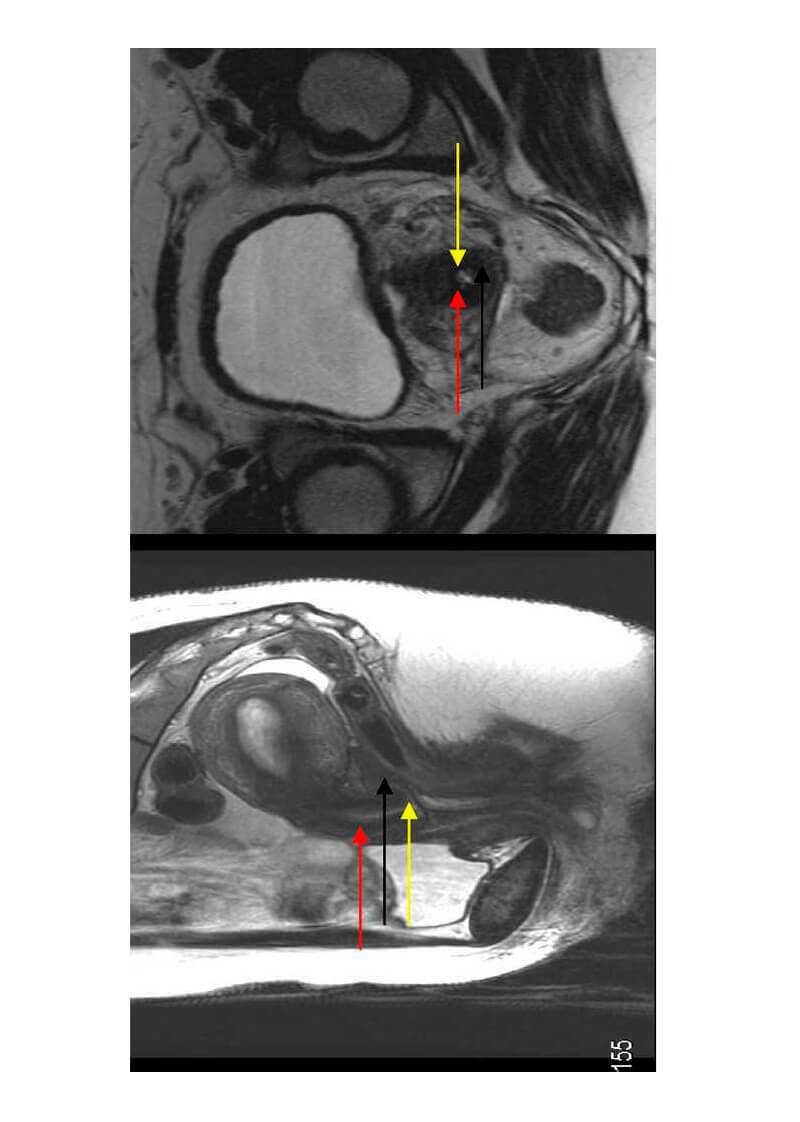
The final decision of the best treatment for each case, in particular, is based on the following variables:
- The tumoral size
- The spread of the disease
- The desire for a future pregnancy
- The general health status
- The patient’s preferences
We are committed to the development of novel surgical techniques for the treatment of gynecologic cancer, including uterine tumors. That said, minimally invasive laparoscopic surgery constitutes the best example of technological development to ensure the best surgical results, minimizing postoperative complications.
Surgical treatment
We are currently especially committed to offering patients the most effective and less invasive therapeutic strategies. Surgical treatment often constitutes the first therapeutic strategy for uterine/endometrial cancer that might include one of the following procedures:
- Hysterectomy: Removal of the uterus including the cervix.
- Bilateral adnexectomy: the removal of both ovaries and the fallopian tubes (uterine adnexa)
- Sentinel lymph node detection: the injection of a tracer (technetium99) in the tumoral region that helps identify the sentinel lymph node in the inguinal region where the tumor would migrate, during the surgical procedure.
This lymph node (although there can be 2 or 3) is identified, removed, and analyzed right then by specialized pathologists. If malignant cells are identified, the removal of all inguinal lymph nodes is carried out. - Aortic and pelvic lymphadenectomy: Removal of the lymph nodes surrounding the main arteries and veins of the abdomen and the pelvis.
- Omentectomy: Removal of the fatty tissue bound to the large intestine. It is reserved for specific types of Endometrial cancer.
After the surgery, the pathologists will assess the sent material carefully to make a final diagnosis and determine the extension of the disease. Afterward, the best postoperative therapeutic option is made based on a series of factors that include:
- The intra-operative findings
- The final histological results
- The general conditions of each patient
- The preferences of the patient and her relatives
The decision can be simple observation and follow-up, or it can rarely include radiotherapy and/or chemotherapy depending on each particular case.
Follow-up and recovery from Endometrial Cancer
The oncologic follow-up period starts after the initial cancer treatment. Its main goal is the early detection of a possible recurrence of the disease.
Beyond adopting effective follow-up rules, we also pay special attention and interest to maintaining and increasing the quality of life of our patients and achieving a rapid and effective re-insertion into their daily life as it was before the cancer diagnosis.
Frequently Asked Questions About Endometrial Cancer
How does endometrial cancer start?
Pelvic pain, a mass, and weight loss
Pelvic pain, feeling a mass (tumor), and unexpected weight loss can also be symptoms of endometrial cancer. These symptoms are usually more common in the later stages of the disease.
How to avoid endometrial cancer?
Can endometrial cancer be prevented?
- Achieve and maintain a healthy weight. …
- Stay physically active. …
- Talk to Dr Lucas Minig about the pros and cons of hormone therapy. …
- Treatment for endometrial problems. …
- Consult with our Specialist if you suffer from HNPCC.
When to suspect endometrial cancer?
The best way to find endometrial cancer early (when it is small) is to see a doctor if you have any signs and symptoms of endometrial cancer, such as abnormal vaginal bleeding or discharge (that is worsening, occurring between periods menstrual
Testimonies of patients with Endometrial Cancer
Doctor Lucas Minig Specialist in Endometrial Cancer in Valencia, Spain
WE WORK FOR YOUR HEALTH

SPECIALIZED TREATMENTS

CONTROL AND DIAGNOSIS

MAXIMUM TECHNOLOGY

Contact the Endometrial Cancer Specialist
Leave us your data and consultation to offer you personalized medical advice
International Consultation
If you want remote medical care, you can consult
through the following links:
International Appointment
Online Consultation
Whatsapp: + 34 679 112 179