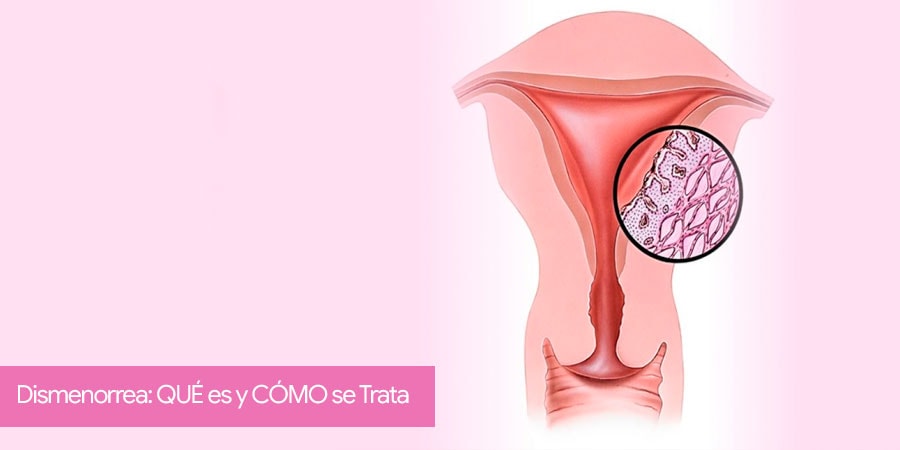
Dysmenorrhea: WHAT is it and HOW is it treated?
Dysmenorrhea is the pain that women experience during their menstrual period, which is the normal vaginal bleeding that happens as part of the hormonal cycle approximately every 28 days.
While many women often present minimal to no pelvic discomfort during their menstrual cycle, some of them can experience very intense pain. Also, there are cases where the pain is so severe it impairs all sorts of daily activities such as going to school/college or work.
In cases where dysmenorrhea alters the quality of life, women must visit a Gynecologist to rule out possible conditions such as ovarian cysts, endometriosis, uterine myomas, or pelvic congestion syndrome. Likewise, treatment strategies can be laid out aiming at reducing pain intensity and thus improving the woman’s queality of life.
How can dysmenorrhea be evaluated?
An important aspect is that the woman visits a Gynecologist as soon as dysmenorrhea starts altering her quality of life. For example, if she has to increase analgesic consumption if it is accompanied by other symptoms like nausea or vomiting, pain during urination or defecation, or leg pain; or if, in more extreme cases, it prevents her from getting out of the house during the day to perform the daily activities.
Typically, dysmenorrhea refers to strong pain in the center of the pelvis (where the uterus is located) that can spread sideways, towards the back, or even to the upper part of the abdomen.
In some women, pain can start progressively some days before the start of the menstrual period until reaching the moment of maximum intensity around days 2 to 3 of the bleeding.
Generally, dysmenorrhea is an unpreventable disease. However, if the woman visits the Gynecologist early, specific strategies can be put in motion aiming at preventing the progression of pain severity throughout the years.
What studies or tests are necessary to evaluate dysmenorrhea?
The main factor is to know how to listen to the patient to understand well if there is any triggering factor and determine the impact it has on her quality of life. Afterward, an exhaustive physical exam must be performed, including a pelvic exam, a gynecologic ultrasound, and, according to the results, a pelvic magnetic resonance (MRI).
In very selected cases and without response to medical treatments (analgesics or hormonal treatments), a diagnostic minimally invasive laparoscopic surgery to directly visualize the pelvic organs.
The purpose of this intervention is to rule out rarer causes that go unnoticed in the mentioned diagnostic studies.
What causes dysmenorrhea?
The causes of dysmenorrhea depend on the type of dysmenorrhea that the patient suffers from primary or secondary dysmenorrhea.
Primary dysmenorrhea
It refers to those women in whom an objective cause is not found and it represents most cases.
Menstrual cramps of primary dysmenorrhea could be explained by a prostaglandin excess, a chemical substance that the uterus produces. Prostaglandins work by contracting and relaxing the uterine muscles, which causes pain/cramps.
Secondary dysmenorrhea
It refers to those cases in which a cause for dysmenorrhea is found. In these cases, the main pathology is endometriosis.
Other less common causes of dysmenorrhea include ovarian cysts, pelvic infection, pelvic congestion syndrome, or intrauterine devices (IUD).
Most effective treatments for dysmenorrhea
There are numerous ways of relieving period cramps. They range from non-pharmacologic treatments such as thermic pads or warm baths, to analgesic drugs of different intensities, under medical prescription.
When the pain is severe enough and analgesics cannot control it, the Gynecologist might request additional studies such as an ultrasound or a pelvic resonance to rule out some conditions such as ovarian cysts, endometriosis, or pelvic congestion syndrome.
In very selected cases with dysmenorrhea progression and lack of response to analgesics, diagnostic laparoscopic surgery might be attempted to directly observe the inside of the pelvis.
Most effective analgesics for dysmenorrhea
Today, there are multiple types of analgesics to alleviate dysmenorrhea. The most common ones are Paracetamol, Ibuprofen, Metamizole (Nolotil ®) o Dexketoprofen (Enantyum ®) orally every 6-8 hours. In more severe cases some of these analgesics can be administered by intramuscular injection occasionally.
A current way of treating dysmenorrhea is by using contraceptives orally as well as with uterine devices (with a hormonal IUD). In this case, the Gynecologist will explain the advantages of each method to alleviate pain.
In any case, if there is pain during the menstrual period that progressively increases, it is advisable to visit a Gynecology specialist for an adequate assessment and treatment.
![[:es]Extirpar Utero no es necesario Extirpar los ovarios[:]](https://drlucasminig.com/en/wp-content/uploads/logotipo-lucas-minig.jpg)
![[:es]Telemedicina Médico remoto en España NOTICIA[:]](https://drlucasminig.com/en/wp-content/uploads/telemedicina-medico-remoto-doctor-espana-lucas-minig.jpg)
![[:es]La quimioterapia hipertérmica intraperitoneal (HIPEC), no es útil en mujeres con cáncer de ovario[:]](https://drlucasminig.com/en/wp-content/uploads/quimioterapia-hipertermica-intraperitoneal-no-util-cancer-de-ovario.jpg)
![[:es]Vacuna Contra VPH reduce cáncer de útero[:]](https://drlucasminig.com/en/wp-content/uploads/vacuna-contra-vph-noticias-dr-lucasminig.jpg)
